80 yr old female with k/c/o type2 DM since 15yrs came with H/o fever associated with chills since 20days,h/o dry cough since 15 days,H/o involuntary dribbling of urine while coughing since 15days,H/o generalised weakness since 4days
This is an online E log book to discuss our patient's de-identified health data shared after taking his/ her /guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Chief complaints:-
80 yr old female with k/c/o type2 DM on OHA and HTN since 15yrs came with
C/o fever associated with chills since 20days,
C/o dry cough since 15 days
C/o involuntary dribbling of urine while coughing since 15days,
C/o generalised weakness since 4days,
Pt was found in unresponsive state, unable to getup, difficulty in speaking, associated with sweating around 8am.Iv fluids were given
By Afternoon, pt was able to speak.
Around 6pm, pt was again found unresponsive associated with sweating , this episode lasted fr 2hrs. RMP was called upon . On checking vitals , BP was found to be 170/70mmhg, and was given antihypertensives , no frothing, no seizures,
She regained consciousness for a while (5min) and again lost consciousness associated with snoring and sweating.
Pt was brought to casuality,
GRBS - 48MG/DL
After 25%D was given, pt became conscious , she could sit and became normal. Her GRBS raised to 231mg/dl after 30min, 2.IV fluids were given,
Pt didn't take food and fluids since 2 days
No H/o headinjury, nausea, Vomitings, blurring of vision, no h/o headache, no h/o involuntary movements, No h/o decreased sensation,
HOPI:-
pt was apparently asymptomatic 20days ago later she had fever associated with chills since 20days which was gradually progressive,
h/o dry cough since 15 days no diurnal variation, no wheeze,,H/o involuntary dribbling of urine while coughing since 15days pale yellow colour,nonfoul smelling
H/o generalised weakness since 4days,
She had decreased food and fluid intake since 10days
Past history:-
NO H/O SIMILAR COMPLAINTS IN THE PAST
H/O DM SINCE 15YRS -
on tab glibenclamide 5mg + t. metformin 500mg
T.,pioglitazone 20mg
H/0 HTN SINCE 15 YRS on tab telma-H (40/12.5mg)
no TB/ASTHMA/EPILEPSY/CAD
-1st may 2020 when she went to hospital with complaint of burning sensation in epigastrium
Rbs
took x ray for knee pain and burning sensation in epigastrium on 5th MayShe went to hospital on 15th May 2020
She went to hospital on 15th sep 2020 with c/o anorexia, dyspepsia and decreased sleep and was medicated with below
Her CBP ON 1/9/2020
17th nov 2020 with complain of epigastric region burning sensation
7th feb 2021
She went to hospital with c/o of sensation of mass in throat
14th feb 2021Past SURGICAL HISTORY
She was hysterctomised 40yrs back for AUB
Personal history
Family history
Drug history
General Examination:
Systemic Examination:
Per abdomen
Patient is conscious, coherent, cooperative;
well oriented to time, place and person.
Hypoactive and drowsy on the day of admission
Speech - normal BUT there is difficulty in speaking on day of admission
Higher mental functions- normal
cranial nerves- intact
motor system- normal
sensory system - normal
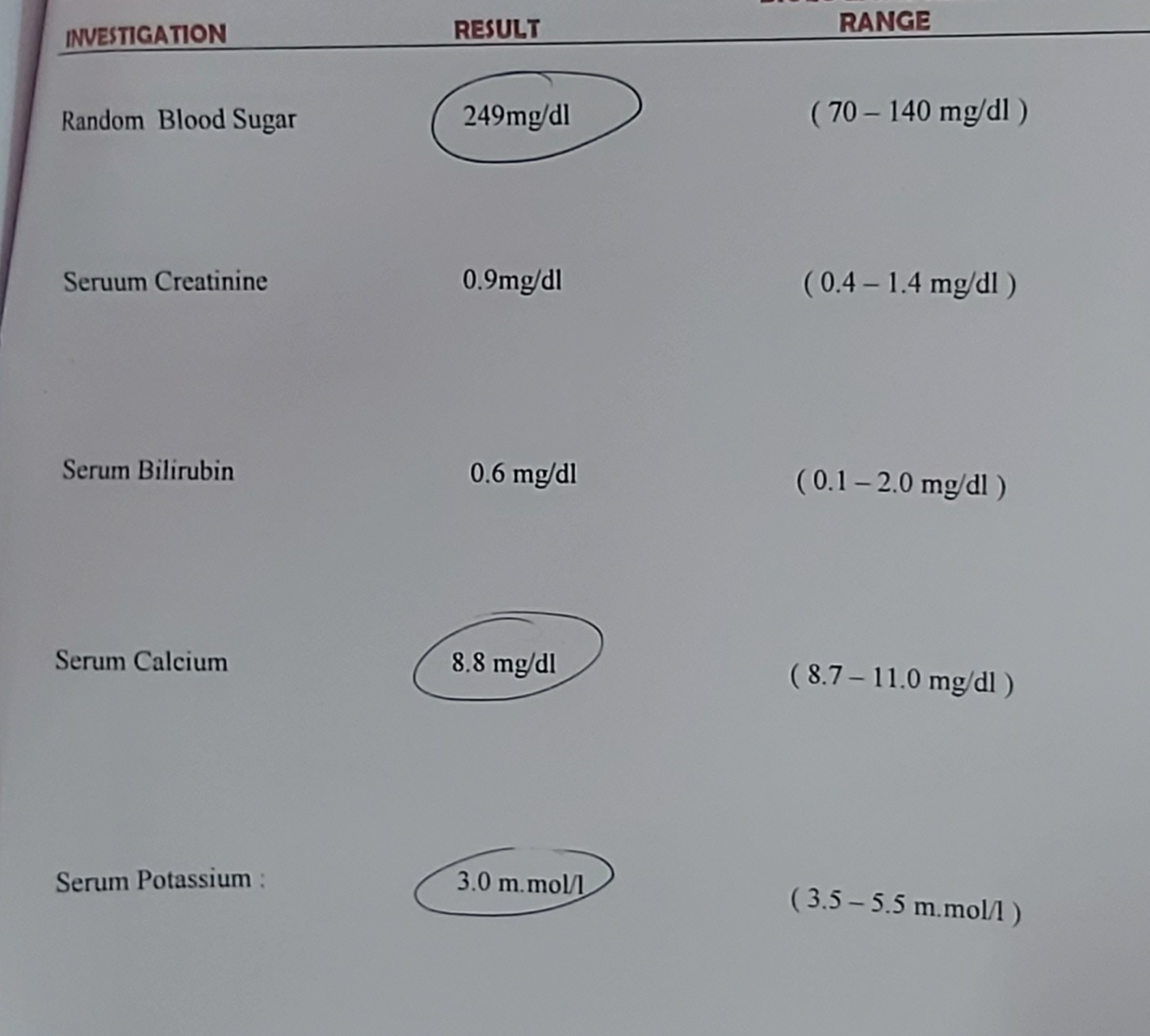
INVESTIGATION:
CBP:
RFT:
Reticulocyte count:-
serum sodium:-24/3
CXR PA VIEW:
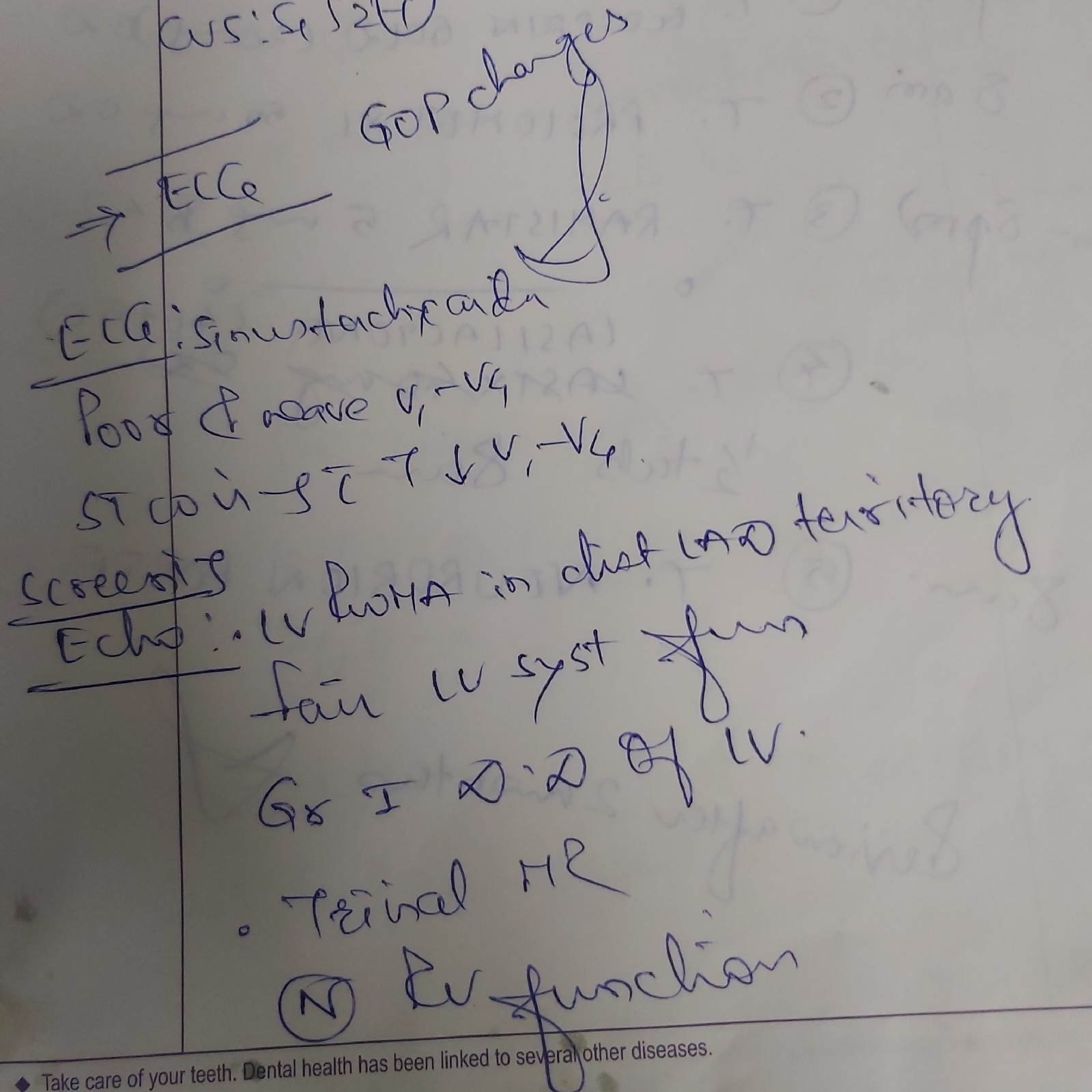
ECG:
Rbs: 143mg/dl
24/3
1:00am 121mg/dl
2:00am:153mg/dl
8:00am 212mg/dl
10:00am 218mg/dl
12:00pm 200mg/dl
2:00pm 246mg/dl
25/3/21
8pm 139mg/dl
10pm 228mg/dl
12am 216mg/dl
2am 172mg/dl
4am 171mg/dl
6am 167mg/dl
8am 167mg/dl
26/3/21
8pm 182mg/dl
10pm 192mg/dl
12am 196mg/dl
2am 186mg/dl
4 am 198mg/dl
6 am 203mg/dl
Usg on 25/3/21
Serum sodium
Esr:-
Diagnosis:-
Recurrent Hypoglycemia-drug induced oha
Fever under evaluation -left lower lobe consolidation
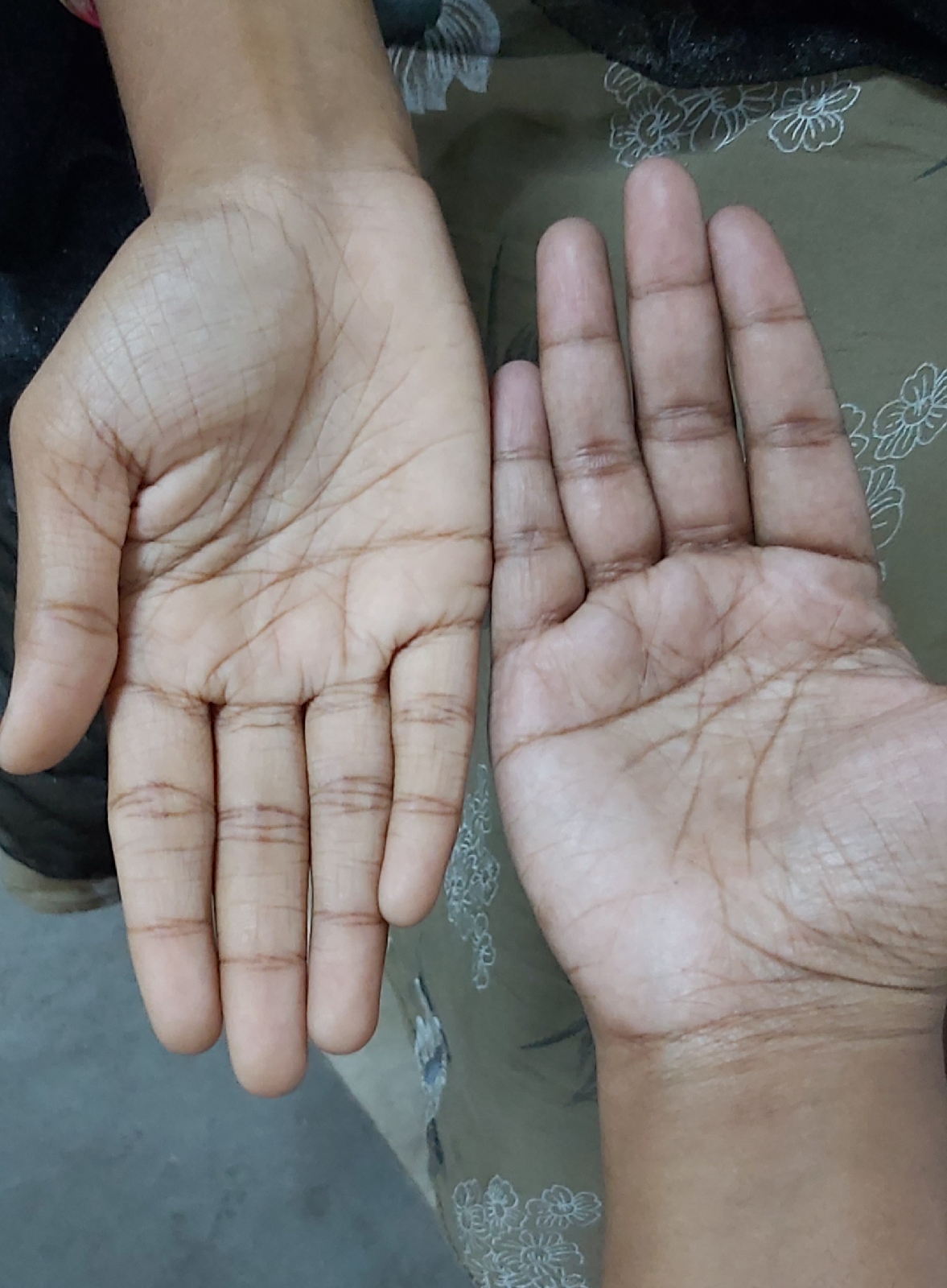
Anemia? IdA
Hypovolemic hyponatremia
k/c/o DM, HTN SINCE 15YRS
TREATMENT:-
PLENTY OF ORAL FLUIDS
1. IVF- 2 . NS @25ML/HR
2. GRBS CHARTING 4TH HRLY
3.BP CHARTING 4TH HRLY
4.TEMP CHARTING 4TH HRLY
5.SYR BENADRYL 10ML/PO/BD(1-X-1)
6.TAB PANTOP 49MG/PO/OD/BBF-8AM
Discussion:-
-Sir his motor weakness is suggestive of predominantly C7 ,C8 nerve involvement along with C6 and T1 also
But no objective sensory involvement.
So most likely is it that the medial cord of the brachial plexus got involved ?
And how to explain his wasting sir of the proximal muscles of left upper limb?
-Wasting with increased tone in left (as mentioned in Sruthi's findings above?
-Yes sir
?Increased tone can be explained with 6 months back CVA and wasting with the long term peripheral neuropathy??
-
If a person with long term peripheral neuropathy develops an upper motor neuron lesion would the previous flaccid tone increase?